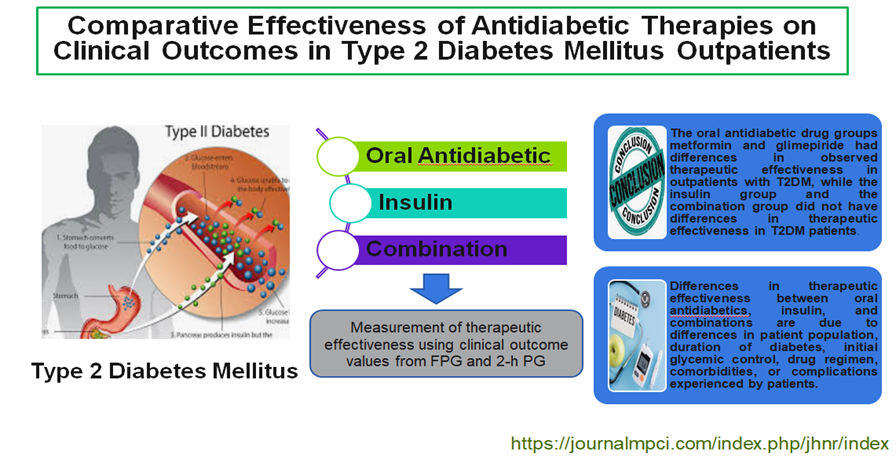
Comparative Effectiveness of Antidiabetic Therapies on Clinical Outcomes in Type 2 Diabetes Mellitus Outpatients
Keywords:
Antidiabetic drug, Effectiveness, Type 2 diabetes mellitusAbstract
This study used observational analysis with retrospective data collection. A total of 303 outpatients with were included in this study. The research instrument used was secondary from medical record data and examination results of Fasting Plasma Glucose (FPG) and 2-hour plasma glucose (2-h PG) values when the patient first visited and the fourth month after the first visit. The patients' therapy is regarded as effective if the FPG test results range from 80-130 mg/dL and the 2-h PG test value is <180 mg/dL in the fourth month. In patients aged >60 years, it is said to be effective if the results of the FPG examination are around ≤ 180 mg/dL and the 2-h PG examination value is ≤200 mg/dL. Data were analyzed using Kruskal-Wallis analysis. Oral antidiabetics metformin and glimepiride had differences in observed effectiveness (p=0.000) < 0.05 for FPG and 2-h PG examinations in outpatients with type 2 diabetes mellitus. The type of oral antidiabetic glimepiride had differences in observed effectiveness (p=0.002) < 0.05 in the FPG examination and (p=0.006) < 0.05 in the 2-h PG examination. The oral antidiabetic drug groups metformin and glimepiride had differences in observed therapeutic effectiveness in outpatients with T2DM, while the insulin group and the combination group did not have differences in therapeutic effectiveness in T2DM patients.
Downloads
References
Davies MJ, Aroda VR, Collins BS, Gabbay RA, Green J, Maruthur NM, et al. Management of Hyperglycemia in Type 2 Diabetes. A Consensus Report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2022;45(11):2753–86. doi:10.2337/dci22-0034.
Padhi S, Nayak AK, Behera A. Type II diabetes mellitus: a review on recent drug based therapeutics. Biomedicine and Pharmacotherapy. 2020;131:110708. doi:10.1016/j.biopha.2020.110708.
Majety P, Alejandra Lozada Orquera F, Edem D, Hamdy O. Pharmacological approaches to the prevention of type 2 diabetes mellitus. 2023;9:14:1118848. doi:10.3389/fendo.2023.1118848.
IDF. Diabetes Atlas 10th edition. International Diabetes Federation; 2021. Available from: www.diabetesatlas.org
RISKESDAS. Hasil Riset Kesehatan Dasar Tahun 2018. Kementrian Kesehatan RI; 2018;53(9):1689–99. Available from: https://layanandata.kemkes.go.id/katalog-data/riskesdas/ketersediaan-data/riskesdas-2018
PERKENI. Pedoman Pengelolaan dan Pencegahan Diabetes Melitus Tipe 2 Dewasa di Indonesia Tahun 2021. Perkumpulan Endokrinologi Indonesia. PB Perkeni. 2021;1-46.
Jamaluddin G, Zulmansyah, Nalapraya WY. Perbandingan Efektivitas Insulin, Obat Antidiabetik Oral dan Kombinasi terhadap Kadar Gula Darah pada Pasien Rawat Jalan dengan DM Tipe 2 RSUD Al-Ihsan. Bandung Conference Series: Medical Science. 2022;2(1):511–6. ISSN: 2828-2205
Ambianti N, Zainal AP, Rumi A, Rezkia K, Tamrin M. Persepsi Pengobatan Terhadap Kepuasan Terapi Pasien Diabetes Mellitus Tipe II. Jurnal Ilmiah Farmasi Farmasyifa. 2024;7(1):1–12. doi:0.29313/jiff.v7i1.2853.
Ghassab-Abdollahi N, Nadrian H, Pishbin K, Shirzadi S, Sarbakhsh P, Saadati F, Moradi MS, Azar PS, Zhianfar L. Gender and Urban–Rural Residency Based Differences In The Prevalence Of Type-2 Diabetes Mellitus and Its Determinants Among Adults In Naghadeh: Results of IraPEN survey. PLoS One. 2023;1(18):1-16. doi:10.1371/journal.pone.0279872.
Estoppey P, Clair C, Auderset D, Puder JJ. Sex Differences In Type 2 Diabetes. Cardiovascular Medicine. 2023;26(3):96–9. doi:10.4414/cvm.2023.02273.
Utomo AA, Aulia A, Rahmah S, Amalia R. Faktor Risiko Diabetes Mellitus Tipe 2 : A Systematic Review. AN-Nur : Jurnal Kajian dan Pengembangan Kesehatan Masyarakat. 2020;01(01):45–52. doi:10.31101/jkk.395.
Tariq JA, Mandokhail KU, Sajjad N, Hussain A, Javaid H, Rasool A, Sadaf H, Javaid S, Durrani AR. Effects of Age and Biological Age-Determining Factors on Telomere Length in Type 2 Diabetes Mellitus Patients. Medicina (Lithuania). 2024 May 1;60(5):698. doi:10.3390/medicina60050698.
RISKESDAS. Laporan_Nasional_Riskesdas 2018. Kementrian Kesehatan Republik Indonesia. Badan Penelitian dan Pengembangan Kesehatan. 2019;1-627. Availeble from : https://repository.badankebijakan.kemkes.go.id/id/eprint/3514/
Lamoia TE, Shulman GI. Cellular and Molecular Mechanisms of Metformin Action. Vol. 42, Endocrine Reviews. Endocrine Society; 2021; 28;42(1):77-96. doi: 10.1210/endrev/bnaa023.
Vashisht R, Patel A, Dahm L, Han C, Medders KE, Mowers R, Byington CL, Koliwad SK, Butte AJ. Second-Line Pharmaceutical Treatments for Patients with Type 2 Diabetes. JAMA Netw Open. 2023;6(10):E2336613. doi:10.1001/jamanetworkopen.2023.36613.
Consoli A, Czupryniak L, Duarte R, Jermendy G, Kautzky-Willer A, Mathieu C, Melo M, Mosenzon O, Nobels F, Papanas N, Roman G, Schnell O, Sotiropoulos A, Stehouwer CDA, Tack CJ, Woo V, Fadini GP. Positioning sulphonylureas in a modern treatment algorithm for patients with type 2 diabetes: Expert opinion from a European consensus panel. Vol. 22, Diabetes, Obesity and Metabolism. Blackwell Publishing Ltd; 2020. 1705–13. doi:https://doi.org/10.1111/dom.14102.
PERKENI. Pedoman Petunjuk Praktis Terapi Insulin Pada Pasien Diabetes Mellitus Tahun 2021. Perkumpulan Endokrinologi Indonesia. PB Perkeni. 2021:1–70.
Davies MJ, D’Alessio DA, Fradkin J, Kernan WN, Mathieu C, Mingrone G, Rossing P, Tsapas A, Wexler DJ, Buse JB. Management of hyperglycemia in type 2 diabetes. A consensus report by the American Diabetes Association (ADA) and the european association for the study of diabetes (EASD). Diabetes Care. American Diabetes Association Inc. 2018;41(12):2669-2701. doi:10.2337/dci18-0033.
Vos RC, van Avendonk MJP, Jansen H, Goudswaard AN, van den Donk M, Gorter K, Kerssen A, Rutten GE. Insulin monotherapy compared with the addition of oral glucose-lowering agents to insulin for people with type 2 diabetes already on insulin therapy and inadequate glycaemic control. Cochrane Database of Systematic Reviews. John Wiley and Sons Ltd. 2016;18;9(9):CD006992. doi: 10.1002/14651858.CD006992.pub2.
Weinberg Sibony R, Segev O, Dor S, Raz I. Drug Therapies for Diabetes. Vol. 24, International Journal of Molecular Sciences. Multidisciplinary Digital Publishing Institute (MDPI); 2023;24(24), 17147. doi:https://doi.org/10.3390/ijms242417147.
Ohishi M. Hypertension with diabetes mellitus: Physiology and pathology review-article. Hypertension Research. 2018;41(6):389–93. doi:10.1038/s41440-018-0034-4.
Przezak A, Bielka W, Pawlik A. Hypertension and Type 2 Diabetes—The Novel Treatment Possibilities. International Journal of Molecular Sciences. MDPI. 2022; 23(12):6500. doi:10.3390/ijms23126500
Abu-Ashour W, Twells L, Valcour J, Randell A, Donnan J, Howse P, Gamble JM. The association between diabetes mellitus and incident infections: A systematic review and meta-analysis of observational studies. BMJ Open Diabetes Res Care. 2017;5(1):e000336. doi: 10.1136/bmjdrc-2016-000336
Inman M, Lyon AW, Lyon OAS, Lyon ME. Estimated risk for insulin dose error among hospital patients due to glucose meter hematocrit bias in 2020. Arch Pathol Lab Med. 2020;144(10):1204-1208. doi:10.5858/arpa.2020-0101-RA.
PERKENI. Pedoman Pemantauan Glukosa Darah Mandiri 2021. Perkumpulan Endokrinologi Indonesia. PB Perkeni. 2021;1-49 p.
Udayani NNW, Meriyani H. Perbedaan Efektivitas Penggunaan Obat Antidiabetik Oral Tunggal Dengan Kombinasi Pada Pasien Dm Tipe 2 Di Upt. Puskesmas Dawan Ii Kabupaten Klungkung Periode November 2015-Pebruari 2016. Jurnal Ilmiah Medicamento. 2016;2(2):47–52. doi:10.36733/medicamento.v2i2.1096.
Bin Rakhis SA, AlDuwayhis NM, Aleid N, AlBarrak AN, Aloraini AA. Glycemic Control for Type 2 Diabetes Mellitus Patients: A Systematic Review. Cureus. 2022; 14(6):e26180. doi:10.7759/cureus.26180
Nigussie S, Birhan N, Amare F, Mengistu G, Adem F, Abegaz TM. Rate of glycemic control and associated factors among type two diabetes mellitus patients in Ethiopia: A cross sectional study. PLoS One. 2021;16(5):e0251506. doi: 10.1371/journal.pone.0251506
Diana K, Amalia Purnamasari Zainal, Setaiawati Fadhilah Zainal, Muhammad Rinaldhi Tandah, Dhea Puspita, Ambianti N. Kegagalan Pengendalian Diabetes Mellitus Tipe Ii Ditinjau Dari Faktor Predisposisi. Jurnal Ilmiah Manuntung. 2024;10(2):178–90. doi: 10.51352/jim.v10i2.886.
Mutmainah N, Al Ayubi M, Widagdo A. Kepatuhan dan Kualitas Hidup Pasien Diabetes Melitus Tipe 2 di Rumah Sakit di Jawa Tengah. Pharmacon: Jurnal Farmasi Indonesia. 2020;17(2):165–73. doi: 10.23917/pharmacon.v17i2.12281.
Published
How to Cite
Issue
Section
Copyright (c) 2025 Muhamad Rinaldhi Tandah, Khusnul Diana, Chairunisah Hidayat, Nurul Ambianti

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Most read articles by the same author(s)
- Muhamad Rinaldhi Tandah, Nurul Ambianti, Yenita Kartika Putri, Khusnul Diana, Development of Drug Plan and Control App Using ABC, VEN, and Combined Methods for Inventory Control , Journal of Health and Nutrition Research: Vol. 4 No. 2 (2025)