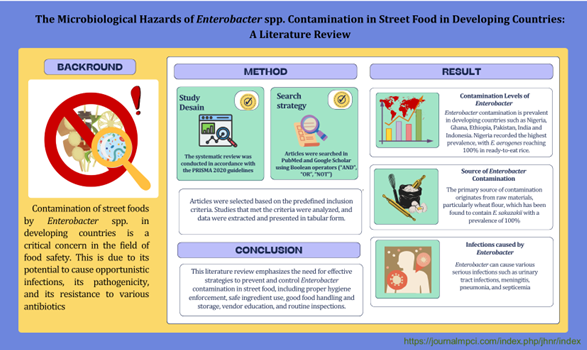
The Microbiological Hazards of Enterobacter spp. Contamination in Street Food in Developing Countries: A Literature Review
Keywords:
Developing countries, Enterobacter, Foodborne, Food safety, Microbiological hazard, Street foodAbstract
Street food is widely consumed by people in developing countries and often poses health risks due to bacterial contamination. The consumption of contaminated food has been linked to more than 200 types of diseases, resulting in 600 million cases and 420,000 deaths each year. One commonly found bacterium is Enterobacter, which can be pathogenic and exhibit resistance to various antibiotics. This review aims to assess the dangers of Enterobacter contamination in street food, including the level and source of contamination, pathogenicity, and management strategies. The review followed PRISMA 2020 guidelines, with literature searches performed in scientific databases such as PubMed and Google Scholar using Boolean operators and relevant keywords. Articles were selected based on specific inclusion criteria, analyzed, and grouped for ease of interpretation. The results showed that Enterobacter contamination is prevalent in developing countries such as Nigeria, Ghana, Ethiopia, Pakistan, India, and Indonesia. Nigeria recorded the highest prevalence, with E. aerogenes reaching 100% in ready-to-eat rice. The primary source of contamination is raw materials, particularly wheat flour, which contains E. sakazakii with a prevalence of 100%. Enterobacter can cause various serious infections, including urinary tract infections, meningitis, pneumonia, and septicemia. Efforts to reduce Enterobacter contamination in street food should include the implementation of hygiene and sanitation practices, the use of safe raw materials, proper processing and storage methods, education for vendors, and routine food safety supervision. These findings are crucial for supporting public health interventions and developing effective food safety policies.
Downloads
References
Mengistu DA, Belami DD, Tefera AA, Alemeshet Asefa Y. Bacteriological quality and public health risk of ready-to-eat foods in developing countries: Systematic review and meta analysis. Microbiology Insights. 2022 Jan;15:117863612211139.
Havelaar AH, Kirk MD, Torgerson PR, Gibb HJ, Hald T, Lake RJ, et al. World Health Organization global estimates and regional comparisons of the burden of foodborne disease in 2010. Von Seidlein L, editor. PLoS Med. 2015 Dec 3;12(12):e1001923.
Lee H, Yoon Y. Etiological agents implicated in foodborne illness world wide. Food Sci Anim Resour. 2021 jan;41(1):1–7.
Barreira MJ, Marcos S, Flores CV, Lopes TT, Moura IB, Correia CB, et al. Microbiological quality of ready-to-eat street foods in Lisbon, Portugal. Discov Food. 2024 Jun 24;4(1):45.
Sabuj AAM, Haque ZF, Younus MdI, Pondit A, Barua N, Hossain MdG, et al. Microbial risk assessment of ready-to-eat fast foods from different street-vended restaurants. Int J One Health. 2020;6(1):41–8.
Lyytinen OL, Dapuliga C, Wallinger D, Patpatia S, Audu BJ, Kiljunen SJ. Three novel Enterobacter cloacae bacteriophages for therapeutic use from Ghanaian natural waters. Arch Virol. 2024 Aug;169(8):156.
Herawati H, Sakati SN, Sumarto Z. Kualitas bakteriologis pada peralatan Makan di Warung Makan Kadompe di Kota Luwuk Kabupaten Banggai. JIK. 2022 Aug 29;16(2):200–6.
Asiegbu CV, Lebelo SL, Tabit FT. Microbial quality of ready-to-eat street vended food groups sold in the Johannesburg Metropolis, South Africa. JFQHC [Internet]. 2020 Feb 27 [cited 2024 Oct 7]; Available from: https://publish.kne-publishing.com/index.php/JFQHC/article/view/2448
Hossain MB, Mahbub NDB, Chowdhury MMK, Rahaman MM. Molecular characterization of Enterobacter and Escherichia coli pathotypes prevalent in the popular street foods of Dhaka City and their multidrug resistance. Bangla J Microbiol. 2019 Jan 1;34(2):67–72.
Dela H, Egyir B, Behene E, Sulemana H, Tagoe R, Bentil R, et al. Microbiological quality and antimicrobial resistance of bacteria species recovered from ready-to-eat food, water samples, and palm swabs of food vendors in Accra, Ghana. International Journal of Food Microbiology. 2023 Jul;396:110195.
Izevbuwa O, Okhuebor S. Microbiological assessment of ready to eat food from selected street vending food locations in Ikpoba-okha local government area of Edo State. BE. 2021 Jan 20;4(1):20–4.
Sonune NA. Assessment of bacteriological quality of street food and their antibiotic profiling. SAR J Pathol Microbiol. 2022 Jul 13;3(4):39–45.
Amare A, Worku T, Ashagirie B, Adugna M, Getaneh A, Dagnew M. Bacteriological profile, antimicrobial susceptibility patterns of the isolates among street vended foods and hygienic practice of vendors in Gondar town, Northwest Ethiopia: a cross sectional study. BMC Microbiol. 2019 Dec;19(1):120.
Murase K. Cytolysin A (ClyA): A Bacterial virulence factor with potential applications in nanopore technology, vaccine development, and tumor therapy. Toxins. 2022 Jan 21;14(2):78.
Hassanin F, Hassan M, Helmy S. Enterobacteriaceae in meat products sold by street vendors. Benha Veterinary Medical Journal. 2015 Dec 1;29(2):74–9.
Igbinosa IH, Beshiru A, Egharevba NE, Igbinosa EO. Distribution of Enterobacteria in Ready-to-eat food in cafeterias and retail food outlets in Benin City: Public health implications. j com med and phc. 2020 aug 28;32(2):80–94.
Wang S, Xiao SZ, Gu FF, Tang J, Guo XK, Ni YX, et al. Antimicrobial susceptibility and molecular epidemiology of clinical Enterobacter cloacae bloodstream isolates in Shanghai, China. Galdiero M, editor. PLoS ONE. 2017 Dec 15;12(12):e0189713.
Ogunyemi A, Buraimoh O, Onuorah N, Ezeugwu S, Odetunde S, Olumuyiwa E. Bacteria associated with contamination of ready-to-eat (RTE) cooked rice in Lagos-Nigeria. Int J Bio Chem Sci. 2016 Feb 5;9(5):2324.
Nyenje ME, Odjadjare CE, Tanih NF, Green E, Ndip RN. Foodborne pathogens recovered from ready-to-eat foods from roadside cafeterias and retail outlets in Alice, Eastern Cape Province, South Africa: Public health implications. IJERPH. 2012 Jul 27;9(8):2608–19.
Sharma I, Mazumdar J. Assessment of bacteriological quality of ready to eat food vended in streets of Silchar city, Assam, India. Indian Journal of Medical Microbiology. 2014 Apr;32(2):169–71.
Budiarso TY, Amarantini C, Prihatmo G, Restiani R, Putri Y, Kindagen V, et al. Detection of coliforms and enteric pathogens in favorite snack food sold in Yogyakarta City: In Yogyakarta, Indonesia; 2021 [cited 2024 Oct 15]. Available from: https://www.atlantis-press.com/article/125953691
Lou X, Si G, Yu H, Qi J, Liu T, Fang Z. Possible reservoir and routes of transmission of Cronobacter (Enterobacter sakazakii) via wheat flour. Food Control. 2014 Sep;43:258–62.
Razzaq R, Farzana K, Mahmood S, Murtaza G. Microbiological analysis of street vended vegetables in Multan City, Pakistan: A Public Health Concern.
Falomir MP, Rico H, Gozalbo D. Enterobacter and Klebsiella species isolated from fresh vegetables marketed in Valencia (Spain) and their clinically relevant resistances to chemotherapeutic agents. Foodborne Pathogens and Disease. 2013 Dec;10(12):1002–7.
Oranusi S, Olorunfemi OJ. Microbiological safety evaluation of street vended ready-to-eat fruits sold in Ota, Ogun state, Nigeria.
Attien P, Dadie T, Sina H, Kouassi CK, Baba-Moussa L. Sanitary risk factors and microbial profile identification by MALDI-TOF of street ready-to-eat meat products contaminants. Int J Res Granthaalayah. 2020 Jun 30;5(12):164–75.
Shiningeni D, Chimwamurombe P, Shilangale R, Misihairabgwi J. Prevalence of pathogenic bacteria in street vended ready-to-eat meats in Windhoek, Namibia. Meat Science. 2019 Feb;148:223–8.
Saksena R, Malik M, Gaind R. Bacterial contamination and prevalence of antimicrobial resistance phenotypes in raw fruits and vegetables sold in Delhi, India. Journal of Food Safety. 2020 Feb;40(1):e12739.
Shayeghi F, Matini E, Rahbar N, Mojri N, Hosseini SS, Abdollahi M, et al. Microbial contamination of kitchen instruments as a minatory to human health.
Haymanot Tasew TA. Contamination of bacteria and associated factors among food handlers working in the student cafeterias of Jimma University main campus, Jimma, South West Ethiopia. Altern Integ Med [Internet]. 2015 [cited 2024 Oct 17];04(01). Available from: http://www.esciencecentral.org/journals/contamination-of-bacteria-and-associated-factors-among-food-handlers-working-in-the-student-cafeterias-of-jimma-university-main-campus-jimma-south-west-ethiopia-2327-5162.1000185.php?aid=40793
Aruwa CE, Ogundare O. Microbiological Quality assessment of pupuru and plantain flours in an urban market in Akure, Ondo State, South Western Nigeria. OALib. 2017;04(08):1–11.
Ceronifrom D. Musculoskeletal postoperative infections due to Enterobacter cloacae complex: A new reality? J Med Microb Diagn [Internet]. 2014 [cited 2024 Oct 29];03(01). Available from: https://www.omicsonline.org/open-access/musculoskeletal-postoperative-infections-due-to-Enterobacter-cloacaecomplex-a-new-reality-2161-0703.1000128.php?aid=21218
Davin-Regli A, Lavigne JP, Pagès JM. Enterobacter spp.: Update on taxonomy, clinical aspects, and emerging antimicrobial resistance. Clin Microbiol Rev. 2019 Sep 18;32(4):e00002-19.
Mbula J, Abdulsalami MS, Vantsawa PA, Onuh K, Ozojiofor UO, Ayodele SB, et al. Isolation and molecular identification of Enterobacter cloacae from pregnant women with urinary tract infections in Biu, North Eastern Nigeria, Borno State. JAMB. 2023 Apr 18;23(5):1–15.
Mezzatesta ML, Gona F, Stefani S. Enterobacter cloacae complex: Clinical impact and emerging antibiotic resistance. Future Microbiol. 2012 Jul;7(7):887–902.
Šín R, Štruncová D, Čechurová L. Clinical picture, diagnostics and treatment of bacterial meningitis.
Yamamoto H, Miyamoto Y, Yamamoto H. A case of bacterial meningitis with burst waves of local onset on ictal Electroencephalography. Pediatrics International. 2019 Dec;61(12):1263–4.
Zhou X, Fu S, Gao J, Chen H. Enterobacter sakazakii: an emerging foodborne pathogenic bacterium. Ann Microbiol. 2012 Mar;62(1):1–5.
Rizi KS. Clinical and pathogenesis overview of Enterobacter infections. 6(4).
Appleberry H, Patel R, Singh K, Wolfe AJ, Putonti C, Kula A. Draft genomes of two Enterobacter hormaechei strains isolated from catheterized urine samples from females experiencing overactive bladder symptoms. Klepac-Ceraj V, editor. Microbiol Resour Announc. 2024 Aug 13;13(8):e00491-24.
Jiménez-Castillo RA, Aguilar-Rivera LR, Carrizales-Sepúlveda EF, Gómez-Quiroz RA, Llantada-López AR, González-Aguirre JE, et al. A case of round pneumonia due to Enterobacter hormaechei: the need for a standardized diagnosis and treatment approach in adults. Rev Inst Med trop S Paulo. 2021;63:e3.
Mohammed MA, Alnour TMS, Shakurfo OM, Aburass MM. Prevalence and antimicrobial resistance pattern of bacterial strains isolated from patients with urinary tract infection in Messalata Central Hospital, Libya. Asian Pacific Journal of Tropical Medicine. 2016 Aug;9(8):771–6.
Westerfeld C, Papaliodis GN, Behlau I, Durand ML, Sobrin L. Enterobacter amnigenus endophthalmitis. Retinal Cases & Brief Reports. 2009;3(4):409–11.
Cruz R, López E, Meneses C, Alegría Y. Bacteriemia por Enterobacter cancerogenus en un paciente con trauma pélvico. Rev chil infectol. 2022 Apr;39(2):218–20.
Demir T, Baran G, Buyukguclu T, Sezgin FM, Kaymaz H. Pneumonia due to Enterobacter cancerogenus infection. Folia Microbiol. 2014 Nov;59(6):527–30.
Berinson B, Bellon E, Christner M, Both A, Aepfelbacher M, Rohde H. Identification of Kosakonia cowanii as a rare cause of acute cholecystitis: Case report and review of the literature. BMC Infect Dis. 2020 Dec;20(1):366.
Chen Q, Lin Y, Li Z, Lu L, Li P, Wang K, et al. Characterization of a new transposon, Tn6696, on a blaNDM–1-Carrying plasmid from multidrug-resistant Enterobacter cloacae ssp. dissolvens in China. Front Microbiol. 2020 Sep 15;11:525479.
Kesieme EB, Kesieme CN, Akpede GO, Okonta KE, Dongo AE, Gbolagade AM, et al. Tension pneumatocele due to Enterobacter gergoviae pneumonia: A case report. Case Reports in Medicine. 2012;2012:1–3.
Satlin MJ, Jenkins SG, Chen L, Helfgott D, Feldman EJ, Kreiswirth BN, et al. Septic shock caused by Klebsiella pneumoniae carbapenemase-producing Enterobacter gergoviae in a neutropenic patient with leukemia. J Clin Microbiol. 2013 Aug;51(8):2794–6.
Manandhar S, Nguyen Q, Pham DT, Amatya P, Rabaa M, Dongol S, et al. A fatal outbreak of neonatal sepsis caused by mcr-10-carrying Enterobacter kobei in a tertiary care hospital in Nepal. Journal of Hospital Infection. 2022 Jul;125:60–6.
Zeng H, Tan Y, Su J, Gao F, Lei T, Liang B. Co-occurrence of blaNDM-1, rmtC, and mcr-9 in multidrug-resistant Enterobacter kobei strain isolated from an infant with urinary tract infection. Journal of Global Antimicrobial Resistance. 2023 Jun;33:221–6.
Shafeeq S, Wang X, Lünsdorf H, Brauner A, Römling U. Draft genome sequence of the urinary catheter isolate Enterobacter ludwigii CEB04 with high biofilm forming capacity. Microorganisms. 2020 Apr 5;8(4):522.
Wagner L, Bloos F, Vylkova S. Bloodstream infection due to Enterobacter ludwigii, correlating with massive aggregation on the surface of a central venous catheter. Infection. 2020 Dec;48(6):955–8.
Kim DM, Jang SJ, Neupane GP, Jang MS, Kwon SH, Kim SW, et al. Enterobacter nimipressuralis as a cause of pseudobacteremia. BMC Infect Dis. 2010 Dec;10(1):315.
Mertschnigg T, Patz S, Becker M, Feierl G, Ruppel S, Bunk B, et al. First report of Kosakonia radicincitans bacteraemia from Europe (Austria) - Identification and whole-genome sequencing of strain DSM 107547. Sci Rep. 2020 Feb 6;10(1):1948.
Rubinstien EM, Klevjer-Anderson P, Smith CA, Drouin MT, Patterson JE. Enterobacter taylorae, a new opportunistic pathogen: Report of four cases. J Clin Microbiol. 1993 Feb;31(2):249–54.
De Vogli R, Kouvonen A, Gimeno D. The influence of market deregulation on fast food consumption and body mass index: A cross-national time series analysis. Bull World Health Organ. 2014 Feb 1;92(2):99-107A.
Verma R, Mishra S. Food safety issues of street foods and dietary practices by school going adolescents.
Weller DL, Ray LC, Payne DC, Griffin PM, Hoekstra RM, Rose EB, et al. An enhanced method for calculating trends in infections caused by pathogens transmitted commonly through food [Internet]. Epidemiology; 2022 [cited 2024 Oct 11]. Available from: http://medrxiv.org/lookup/doi/10.1101/2022.09.14.22279742
Holland D, Thomson L, Mahmoudzadeh N, Khaled A. Estimating deaths from foodborne disease in the UK for 11 key pathogens. BMJ Open Gastroenterol. 2020 Jun;7(1):e000377.
Majeed A. Food toxicity: Contamination sources, health implications and prevention.
Micheel V, Hogan B, Rakotoarivelo R, Rakotozandrindrainy R, Razafimanatsoa F, Razafindrabe T, et al. Identification of nasal colonization with β-lactamase-producing Enterobacteriaceae in patients, health care workers and students in Madagascar. European Journal of Microbiology and Immunology. 2015 Mar;5(1):116–25.
Mehboob A, Abbas T. Evaluation of microbial quality of street food in Karachi City, Pakistan: An epidemiological study. Microbiol Res (Pavia) [Internet]. 2019 Jan 29 [cited 2024 Oct 2];10(1). Available from: https://www.pagepress.org/journals/index.php/mr/article/view/7463
Asiegbu CV, Lebelo SL, Tabit FT. The food safety knowledge and microbial hazards awareness of consumers of ready-to-eat street-vended food. Food Control. 2016 Feb;60:422–9.
Raza J, Asmat TM, Mustafa MZ, Ishtiaq H, Mumtaz K, Jalees MM, et al. Contamination of ready-to-eat street food in Pakistan with Salmonella spp.: Implications for consumers and food safety. International Journal of Infectious Diseases. 2021 May;106:123–7.
Akinde SB, Sunday AA, Adeyemi FM, Fakayode IB, Oluwajide OO, Adebunmi AA, et al. Microbes in irrigation water and fresh vegetables: Potential pathogenic bacteria assessment and implications for food safety. Appl Biosaf. 2016 Jun;21(2):89–97.
Mladenović KG, Grujović MŽ, Kiš M, Furmeg S, Tkalec VJ, Stefanović OD, et al. Enterobacteriaceae in food safety with an emphasis on raw milk and meat. Appl Microbiol Biotechnol. 2021 Dec;105(23):8615–27.
Pintor-Cora A, Alegría Á, Ramos-Vivas J, García-López ML, Santos JA, Rodríguez-Calleja JM. Antimicrobial-resistant Enterobacter cloacae complex strains isolated from fresh vegetables intended for raw consumption and their farm environments in the Northwest of Spain. LWT. 2023 Oct;188:115382.
Umar Mustapha M, Halimoon N, Wan Johari WL, Abd Shukor MohdY. Enhanced carbofuran degradation using immobilized and free cells of Enterobacter sp. Isolated from Soil. Molecules. 2020 Jun 16;25(12):2771.
Amare A, Eshetie S, Kasew D, Moges F. High prevalence of fecal carriage of extended-spectrum beta-lactamase and carbapenemase-producing Enterobacteriaceae among food handlers at the University of Gondar, Northwest Ethiopia. Algammal AM, editor. PLoS ONE. 2022 Mar 17;17(3):e0264818.
Khurana KM, Hassani US. Presence of pathogenic Enterobacteriaceae on fingertips of food handlers. Journal of Datta Meghe Institute of Medical Sciences University. 2024 Apr;19(2):281–5.
Moges Tiruneh MD. Bacterial Profile and antimicrobial susceptibility pattern among food handlers at Gondar University Cafeteria, Northwest Ethiopia. J Infect Dis Ther [Internet]. 2013 [cited 2024 Oct 17];01(02). Available from: http://www.esciencecentral.org/journals/bacterial-profile-and-antimicrobial-susceptibility-pattern-among-food-handlers-at-gondar-university-cafeteria-northwest-ethiopia-2332-0877.1000105.php?aid=14902
Zaglool D, Khodari Y, Othman RAM, Farooq M. Prevalence of intestinal parasites and bacteria among food handlers in a tertiary care hospital. Niger Med J. 2011;52(4):266.
Bolourchi N, Fereshteh S, Noori Goodarzi N, Badmasti F. Subtractive genomic analysis for computational identification of putative immunogenic targets against clinical Enterobacter cloacae complex. Marsano RM, editor. PLoS ONE. 2022 Oct 13;17(10):e0275749.
Ben Said L, Jouini A, Klibi N, Dziri R, Alonso CA, Boudabous A, et al. Detection of extended-spectrum beta-lactamase (ESBL)-producing Enterobacteriaceae in vegetables, soil and water of the farm environment in Tunisia. International Journal of Food Microbiology. 2015 Jun;203:86–92.
Nisa TT, Sugawara Y, Hamaguchi S, Takeuchi D, Abe R, Kuroda E, et al. Genomic characterization of carbapenemase-producing Enterobacterales from Dhaka food markets unveils the spread of high-risk antimicrobial-resistant clones and plasmids co-carrying bla NDM and mcr-1.1. JAC-Antimicrobial Resistance. 2024 Jul 3;6(4):dlae124.
Rane S. Street vended food in developing world: Hazard analyses. Indian J Microbiol. 2011 Jan;51(1):100–6.
Grimont F, Grimont PAD. The genus Enterobacter. In: Dworkin M, Falkow S, Rosenberg E, Schleifer KH, Stackebrandt E, editors. The Prokaryotes [Internet]. New York, NY: Springer New York; 2006 [cited 2024 Oct 31]. p. 197–214. Available from: http://link.springer.com/10.1007/0-387-30746-X_9
Haiko J, Westerlund-Wikström B. The role of the bacterial flagellum in adhesion and virulence. Biology. 2013 Oct 25;2(4):1242–67.
Barnes AI, Ortiz C, Paraje MG, Balanzino LE, Albesa I. Purification and characterization of a cytotoxin from Enterobacter cloacae. Can J Microbiol. 1997 Aug 1;43(8):729–33.
Krzymińska S, Mokracka J, Koczura R, Kaznowski A. Cytotoxic activity of Enterobacter cloacae human isolates. FEMS Immunol Med Microbiol. 2009 Aug;56(3):248–52.
Horna G, Ruiz J. Type 3 secretion system of Pseudomonas aeruginosa. Microbiological Research. 2021 May;246:126719.
Hernández-Martínez G, Ares MA, Rosales-Reyes R, Soria-Bustos J, Yañez-Santos JA, Cedillo ML, et al. The nucleoid protein HU positively regulates the expression of type VI secretion systems in Enterobacter cloacae. D’Orazio SEF, editor. mSphere. 2024 May 29;9(5):e00060-24.
Krzymińska S, Koczura R, Mokracka J, Puton T, Kaznowski A. Isolates of the Enterobacter cloacae complex induce apoptosis of human intestinal epithelial cells. Microbial Pathogenesis. 2010 Sep;49(3):83–9.
Paauw A, Caspers MPM, Schuren FHJ, Leverstein-van Hall MA, Delétoile A, Montijn RC, et al. Genomic diversity within the Enterobacter cloacae Complex. Redfield RJ, editor. PLoS ONE. 2008 Aug 21;3(8):e3018.
Paauw A, Caspers MPM, Leverstein-van Hall MA, Schuren FHJ, Montijn RC, Verhoef J, et al. Identification of resistance and virulence factors in an epidemic Enterobacter hormaechei outbreak strain. Microbiology. 2009 May 1;155(5):1478–88.
Royer G, Clermont O, Marin J, Condamine B, Dion S, Blanquart F, et al. Epistatic interactions between the high pathogenicity island and other iron uptake systems shape Escherichia coli extra-intestinal virulence. Nat Commun. 2023 Jun 20;14(1):3667.
Shan C, Liu C, Lu Q, Fu G, Shah SAH, Akhtar RW, et al. High pathogenicity island (HPI) main structural genes and their bioinformatics analysis in clinically isolated E. coli from Saba Pigs. PJZ [Internet]. 2022 [cited 2024 Nov 1];55(2). Available from: http://researcherslinks.com/current-issues/High-Pathogenicity-Island-HPI-Main-Structural-Genes/20/1/5674/html
Souza Lopes AC, Rodrigues JF, Cabral AB, Da Silva ME, Leal NC, Da Silveira VM, et al. Occurrence and analysis of irp2 virulence gene in isolates of Klebsiella pneumoniae and Enterobacter spp. from microbiota and hospital and community-acquired infections. Microbial Pathogenesis. 2016 Jul;96:15–9.
Kim SM, Lee HW, Choi YW, Kim SH, Lee JC, Lee YC, et al. Involvement of curli fimbriae in the biofilm formation of Enterobacter cloacae. J Microbiol. 2012 Feb;50(1):175–8.
Azevedo PAA, Furlan JPR, Oliveira-Silva M, Nakamura-Silva R, Gomes CN, Costa KRC, et al. Detection of virulence and β-lactamase encoding genes in Enterobacter aerogenes and Enterobacter cloacae clinical isolates from Brazil. Brazilian Journal of Microbiology. 2018 Nov;49:224–8.
El Fertas-Aissani R, Messai Y, Alouache S, Bakour R. Virulence profiles and antibiotic susceptibility patterns of Klebsiella pneumoniae strains isolated from different clinical specimens. Pathologie Biologie. 2013 Oct;61(5):209–16.
Claeys G, De Baere T, Wauters G, Vandecandelaere P, Verschraegen G, Muylaert A, et al. Extended-spectrum β-lactamase (ESBL) producing Enterobacter aerogenes phenotypically misidentified as Klebsiella pneumoniae or K. terrigena. BMC Microbiol. 2004 Dec 24;4(1):49.
Davin-Regli A, Pagès JM. Enterobacter aerogenes and Enterobacter cloacae; versatile bacterial pathogens confronting antibiotic treatment. Front Microbiol [Internet]. 2015 May 18 [cited 2024 Nov 1];6. Available from: http://www.frontiersin.org/Antimicrobials%2c_Resistance_and_Chemotherapy/10.3389/fmicb.2015.00392/abstract
Madilo FK, Islam MN, Letsyo E, Roy N, Klutse CM, Quansah E, et al. Foodborne pathogens awareness and food safety knowledge of street-vended food consumers: A case of university students in Ghana. Heliyon. 2023 Jul;9(7):e17795.
Jambre KGE, Lagorra MJP. Compliance to sanitation standard operating procedures: An evaluation of street food handlers in Dipolog City, Philippines. 2022;(6).
Huynh-Van B, Vuong-Thao V, Huynh-Thi-Thanh T, Dang-Xuan S, Huynh-Van T, Tran-To L, et al. Factors associated with food safety compliance among street food vendors in Can Tho city, Vietnam: implications for intervention activity design and implementation. BMC Public Health. 2022 Dec;22(1):94.
Published
How to Cite
Issue
Section
Copyright (c) 2025 Jefyne Mali’ Pareakan, Charis Amarantini, Tri Yahya Budiarso

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.